In this article, we endeavour to present an overview of the current state of affairs regarding the application of Aquatic Therapy in the elderly. We will quote a number of recent articles reporting Aquatic Therapy to:
- Improve the experience of embodiment
- Reduce the symptoms of dementia (although for a short while)
- Alleviate the symptoms of Alzheimer’s Disease
All research efforts we are quoting are real and can be verified in the original articles. For this, please follow the links at the bottom of this page.
Personal note from the author:
At EWAC Medical, we strive to improve the quality of life of the people that use our equipment. Ageing of the human body comes with complaints and aches. Unfortunately, in a staggering amount of cases, age is also a debilitating disease. Many causes of these problems can be named. Some point to higher livings standards and better healthcare causing people to become older so that mental diseases come into view that would otherwise not be seen. Others point to our Western lifestyle including the food we eat or changes in our natural environment. We just don’t know. We prefer to demonstrate how we can support. In some cases, only a little bit, and in others, we may make a huge difference using Aquatic Therapy.
~ Eric Legdeur

Embodiment
We may be inclined to think of our brain as a distinct organ from the body. In that circumstance, the important link between the body and the brain, the source of inputs and learning, is disregarded. There is undeniable interconnectedness between the brain and the body. The brain requires the body to maintain it, and the body requires the brain to direct it. This is how we perceive the world: the brain turns body sensations into a useful set of instructions that allows us to interact with our surroundings. Disconnected from the body (that is, dis-embodied), one may expect the brain to be unable to generate anything from the nonexistent external stimuli, causing it to “drift” away like an incorrectly calibrated compass.
Proponents of the embodied cognition thesis emphasize the active and significant role the body plays in the shaping of cognition and the understanding of an agent’s mind and cognitive capacities. In philosophy, embodied cognition holds that an agent’s cognition, rather than being the product of mere (innate) abstract representations of the world, is strongly influenced by aspects of an agent’s body beyond the brain itself. Thus, the embodiment thesis intends to reintroduce an agent’s bodily experiences into any account of cognition. It is a rather broad thesis and encompasses both weak and strong variants of embodiment. In their attempt to reconcile cognitive science with human experience, Varela et al.’s enactive approach to cognition defines “embodiment” as follows:~source: Wikipedia 2021

“By using the term embodied we mean to highlight two points: first that cognition depends upon the kinds of experience that come from having a body with various sensorimotor capacities, and second, that these individual sensorimotor capacities are themselves embedded in a more encompassing biological, psychological and cultural context.” ~Francisco J. Varela, Evan Thompson, Eleanor Rosch : The Embodied Mind: Cognitive Science and Human Experience pages 172–173
How water and embodiment are related
In a broader sense, the human race transitioned from an aquatic creature to a land creature, and hence the ‘memory’ of immersion in water is ‘ingrained’ in our genes. As a result for example, the body produces a neurological reaction while redistributing blood throughout the body. Aquatic treatment has been proven to improve numerous cognitive subdomains.
As a result, water immersion aids the embodiment process in a variety of ways. It briefly relieves us of the impacts of gravity, making us more comfortable in our bodies. This means that we can address human embodiment in the water at a young age and answer any demands that arise during our birth journey.
Dementia
Dementia manifests as a set of related symptoms, which usually surface when the brain is damaged by injury or disease. The symptoms involve progressive impairments to memory, thinking, and behaviour, which negatively impacts a person’s ability to function and carry out everyday activities. Aside from memory impairment and disruption in thought patterns, the most common symptoms include emotional problems, difficulties with language, and decreased motivation. Dementia is not a disorder of consciousness, and consciousness is not usually affected. ~source: Wikipedia 2021
Alzheimer’s disease
Alzheimer’s disease also referred to simply as Alzheimer’s, is a neurodegenerative disease that usually starts slowly and progressively worsens. It is the cause of 60–70% of cases of dementia. The most common early symptom is difficulty in remembering recent events. As the disease advances, symptoms can include problems with:
- language
- disorientation (including easily getting lost)
- mood swings
- loss of motivation
- self-neglect
- behavioral issues
As a person’s condition declines, they often withdraw from family and society. Gradually, bodily functions are lost, ultimately leading to death. Although the speed of progression can vary, the typical life expectancy following diagnosis is three to nine years. ~source: Wikipedia 2021
The decay of the brain
Following the definitions above, it is possible to conclude that dementia is caused by brain injury. As a result, dementia can appear at any age because a brain injury might occur as a result of an accident in one’s life. The brain, on its own, decays slowly with age, resulting in an ever-increasing number of naturally occurring flaws, which eventually manifest in the person’s behavior.
Promoting factors, mechanisms and diagnosis of Alzheimer’s disease
The exact causes of Alzheimer’s disease are poorly understood. It seems to be a specific expression of damage to the brain that progresses more quickly than is the case in other ageing individuals.
Promoting factors of Alzheimer’s disease:
- brain injury
- clinical depression
- high blood pressure
Mechanism in developing Alzheimer’s disease:
- Formation of Amyloid plaques
- Appearance of Neurofibrillary tangles
- Chronic (neuro) inflammation
- Bad vascular condition
Diagnosis of Alzheimer’s disease:
- Memory impairment
- Difficulty concentrating, planning or problem-solving
- Problems finishing daily tasks
- Confusion with location or passage of time
- Language (word finding) problems
- Poor judgement in decisions
- Withdrawal from work events or social engagements
- Changes in mood, depression and other personality traits
Prevention and treatment of Alzheimer’s disease
The ways in which Alzheimer’s disease can be prevented are not yet entirely clear.
Delaying the onset and treatment op Alzheimer’s disease:
- Social engagement
- Keeping the brain active
- Good and healthy nutrition
- Physical activity
- Physiotherapy
- Aquatic therapy
- Medication (still in first stages of development)

Aquatic Therapy in Alzeheimer’s disease
Quoting the Alzheimer’s Research & Prevention Foundation, ““Get moving: Regular exercise can reduce your risk by up to 50 percent. Studies show that women from ages 40 to 60 who exercised regularly demonstrated a profound reduction in cognitive decline and memory loss.” Regular physical exercise can prevent Alzheimer’s disease by up to 50 percent, according to the Alzheimer’s Research & Prevention Foundation. This is because it helps to stimulate the brain’s capacity for maintaining memories while making new ones.
Aquatic Therapy is also known as:
- Pool therapy
- Aqua therapy
- Hydrotherapy
- Aquatic rehabilitation
- Therapeutic aquatics
- Water therapy
In Alzheimer’s disease, Aquatic Therapy is helpful for:
- Embodiment / re-embodiment
- Aiding locomotion
- Improving balance and coordination
- Building muscle strength
- Improving gait
- Enhancing aerobic capacity
- Improving flexibility of joints and spine
- Promoting of relaxation
- Reducing stress
- Strengthening endurance
Aquatic Therapy therapeutic goals in Alzheimer’s patients
- Activating connectivity between large-scale networks (attentional network, default mode network and others)
- attentional network with executive functions like problem solving, concentration, work memory during motor control tasks (fall prevention)
- default mode network with reflection on the self, which results in re-embodiment
- enhancing cerebral blood flow and addressing neuroinflammation by light aerobic activities
How Aquatic Therapy helps Alzheimer’s patients
Aquatic therapy offers the perfect safe and low impact environment for Alzheimer’s patients to get active and to reduce the progression of their symptoms:
- Keeps them physically active
The biggest problem for Alzheimer’s patients is to stay physically engaged while remaining safe. Many people struggle in larger exercise classes, have a fear of falling, or are unable to participate in non-aquatic fitness activities owing to pain. Hydrotherapy is an excellent answer since it allows them to get the exercise they need to retain strength and balance while also slowing the advancement of their Alzheimer’s symptoms. The low-impact nature of the training regimen reduces worries about losing balance or falling. - Has a relaxing effect on mind and body
Most importantly, aquatic therapy is both naturally calming and challenging. Not only does it relieve tension in the body by reducing joint stress, but the warmth and buoyancy of the water is also proven to relax the mind. Physical activity and distraction from difficult chores help to ease the stress that many Alzheimer’s sufferers endure. Their brain is also activated at the same moment. - Provides opportunities for socialisation
Aquatic therapy is a collaborative exercise that involves both verbal and physical interaction with a therapist. Furthermore, it can be done individually or in groups. In any modality, the sessions provide Alzheimer’s patients with the necessary social connections to stimulate the brain, as well as the opportunity to socialize with people while gaining vital exercise. - Stimulates greater functional mobility
Hydrotherapy not only promotes higher functional movement outside of the water, but it also helps Alzheimer’s patients improve their balance and gait. Clinical trials have shown that patients who participate in aquatic therapy improve their trunk balance, range of motion, and stamina. Their balance is also enhanced as they transition from sitting to standing and vice versa. - Supports the development of a routine
One reason why water therapy may be beneficial to dementia sufferers is that routines are necessary for the brain. Daily or regularly planned water therapy sessions can help patients develop this sense of routine, allowing them to reap the benefits of a consistent schedule. Patients at all stages of Alzheimer’s disease benefit from regularly scheduled activities, which help to reduce the frequency and duration of outbursts.
Case reports
In the following section we will describe two singular case reports as well as a case report describing ten adults, 88 years of age.
Case 1: 54-year old female, former Physiotherapist, Alzheimer’s
Symptoms last 6 months
- Non-verbal
- Transfer assistance required
- Daily living support required
Intervention
- 17 one hour therapy sessions over 19 weeks
Progression after intervention
- Able to tread water for 15 minutes
- Transfers minimally assisted
- Verbal communication improved to appropriate responses

Explanation of effect mechanisms indicated by the researchers
- Aquatic immersion produces significant alterations in the cardiovascular system, resulting in an increase in cardiac output and a decrease in peripheral vascular resistance.
- There is also a neurophysiologic autonomic alteration in sympathovagal balance produced during warm water immersion, as described in papers assessing cardiac vagal control.
- Increase of cardiac output and cerebral blood flow
- The role of exercise in the preservation and improvement of cognitive function is becoming well established science.
- There is an emerging body of literature demonstrating clinical benefits from participation in an aquatic exercise program in mild to moderate Alzheimer’s disease.
Relevant anecdotal evidence indicated by the researchers
- The initial sessions in the 32°C heated pool were significant for a dramatic reduction in agitation and facial expressions of anger with increased verbalization, including her calling out, “Hi Mom,” to her mother who was present in the pool during the therapy session, which she had not done in over a year
- Over the months of her treatment and even following that period, her mother reported that her improved communication skills persisted. She demonstrated consistent yes/no response accuracy, and social comments such as appropriate “thank you” and “very nice” comments recurring as well as other appropriate verbalization
- On her second pool visit she was able to exit the pool via a ramp walking 20’ with minimum (Min) to moderate (Mod) assist
- Also by the 6th visit, the patient began to show ability to tread water, initially for a few seconds but later for minutes, achieving ultimately 15 minutes per session.
- She gained ability to stand upright from a water-treading position, and then to walk, but preferred to swim and tread water
- During her therapy visits no adverse events occurred.
Case 2: 89-year old male, diagnosed with advanced Alzheimer’s
Symptoms
- Incapable of activities of daily living (ADL’s), except to self-feed
- Poorly communicative and expressionless
- Failing conventional physiotherapy
Intervention
- 30 minutes of Aquatic Therapy twice weekly over 3 months
Progression after intervention
- Mini-Mental State Examination (MMSE) improvement from 2/30 to 4/30
- Anecdotal: The examiner noted that he was clearly more expressive and talkative than he was during his baseline MMSE examination.
- Fall risk scores trended downward
Explanation of effect mechanisms indicated by the researchers
- Balance: Buoyancy in the water and the viscosity of water compared with air enable nonambulatory persons and those at high risk of falls to practice balancing skills while strength- ening their lower extremity musculature without the risk of falling.
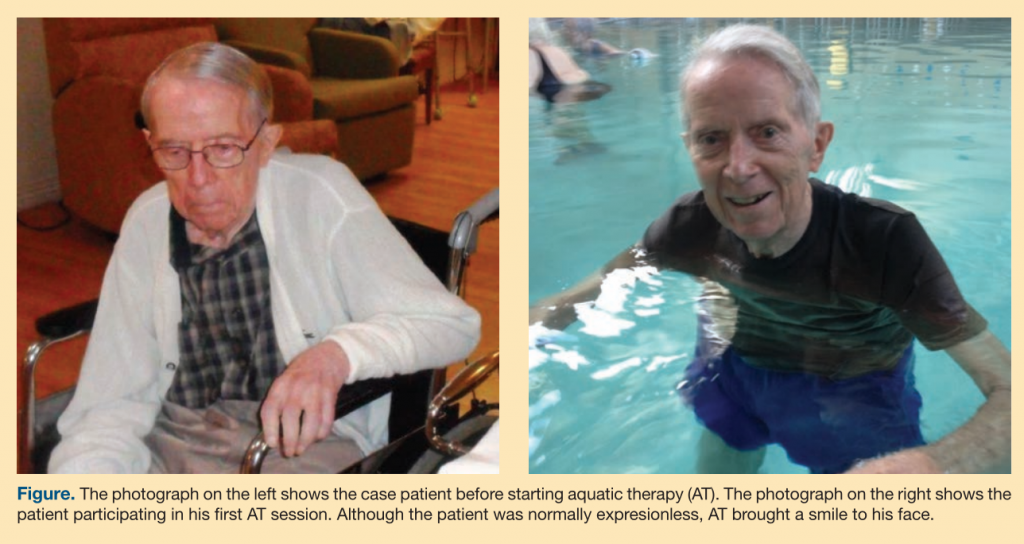
Relevant anecdotal evidence indicated by the researchers
- They also noticed that for 2 to 3 hours after his AT sessions he was smiling more and talking more clearly without his usual trouble finding words. He even joked with the staff.
- In addition, although the case patient was seated and submerged in warm water to his mid-abdomen twice weekly to be bathed, this had no noticeable effect on his cognition, expression, or communication skills; therefore, the mere act of being in the water did not improve his abilities.
- However, his very first AT session brought a broad smile to his normally expressionless face as he realized that he could ambulate in the water and perform AT rhythmic walking and positioning maneuvers
- The patient continued to perform AT exercises at increasingly advanced levels over the subsequent 3 months, and he eventually could obey a command to walk in the water to the edge of the pool, retrieve a pool toy, and bring it back to the aquatic therapist
- His daughter visited him after 2 months of AT and she was also amazed when she got into the pool with him for a session. She stated, “In a way it was like having our dad back. It was amazing that he could communicate, speak in sentences, and follow directions. He really proved that he could understand.”
Case 3: Ten adults, 88-year old, suffering from dementia
This investigation revolved around the feasibility of a dementia-specific aquatic exercise program for nursing home residents with a particular focus on the physical and functional benefits.
General contemporary insights
- A body of research is emerging showing exercise and physical activity has potency as a preventative to dementia.2,3 Specifically, among those who walk greater distance per day or have demonstrated higher physical capacity and muscle strength, the risk of the development of dementia is reduced significantly.
- Anecdotal evidence suggests that for those with dementia, water based exercise has significant behavioral and psychological benefit, with reports suggesting reduced wandering and improved social interactions and sleeping patterns.


Inclusion criteria
- >65 years of age; residing in a nursing home; with a diagnosed dementia and a past history of swimming.
Exclusion criteria
- Residents were excluded if they were: wheelchair bound; had unpredictable or dangerous behaviors; or exercise contraindications; or were unable to stand or walk without assistance of another for a minimum of 6 m.
Intervention
- The Watermemories Swimming Club intervention is a dementia specific, aquatic exercise program designed by an accredited exercise physiologist in consultation with dementia experts. The program incorporates a short walking warm-up and flexibility cool-down, between which participants undertake targeted exercises to improve aerobic, balance, and strength capacity.
Reported benefits of Aquatic Therapy
- A significant improvement in left hand grip strength was found post-intervention (Effect size (r) ¼ 0.53; p ¼ .017). In addition, positive non-significant trends where observed for percent body fat (r ¼ 0.32; p ¼ .154), lean mass (r ¼ 0.23; p ¼ .314), right hand grip strength (r ¼ 0.36; p ¼ .106), standing
- This work compliments previous evidence that aquatic exercise can have important psychological and behavioral implications for institutionalized adults with dementia.
- Our work supports previous anecdotal evidence reporting that swimming exercise can be beneficial for those with dementia,
- Strong benefits, but at the same time lots of practical constraints which prevent real life application of AT in this patient group
Explanation of effect mechanisms indicated by the researchers
- In contrast to land based exercise, our aquatic program is more suitable for those with joint and balance issues and who require low impact training. Specifically, by being in water there is a reduced risk of a falls injury and with an added benefit of resistance. In addition, by using in-pool lane rope or the pool edge, participants could move freely at a moderate intensity while still maintaining a higher level of safety than if involved in, for example, a walking program. Importantly, participants always appeared happy and laughing while participating, which supports previous reduced behavioral symptoms evidence.
- Physical activity is a primary unmet need among those with dementia; interventions that can improve capacity in activities of daily living and prolong wellbeing warrant investigation.
Conclusions:
Embodiment
The notion of embodiment, in the way is described in this article is a relatively recent philosophical insight. This new insight is bound to have it’s impact on medical science, as well as theories of the mind and consciousness. Immersion in water can support the bodily awareness and promote the feeling of embodiment.
Dementia / Alzheimer’s
Dementia / Alzheimer’s are debilitating diseases for which, as of now, there is no cure. Certain medicins though can slow down the onset of these diseases. As this article shows, patients can benefit tremendously from aquatic physical exercise interventions. In the water the sense of embodiment is raised, as is mental clarity. This leads to radical (though temporary) improvements in the behavior and abilities of patients.
Free download links:
Case 1: 54-year old female, former Physiotherapist, Alzheimer’s
Case 2: 89-year old male, diagnosed with advanced Alzheimer’s
Case 3: Ten adults, 88-year old, suffering from dementia


